Scientists have made great strides in cataloguing the human microbiome, the collection of tiny organisms that live on and in our bodies. Now some researchers want to put those microbes to work.
At the forefront of this effort is Jeff Tabor, a synthetic biologist in the Department of Bioengineering at Rice University in Houston. Recently, Tabor received a three-year grant from the Office of Naval Research to genetically modify a strain of Escherichia coli bacteria that lives naturally in the human gut.
The ultimate goal is to create a microbe that can detect and treat an intestinal disorder that has been linked to obesity and depression.
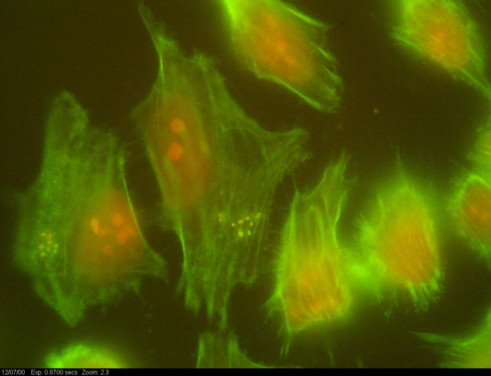
Tabor has been getting microbes to do his bidding since 2004, when he helped create a living photographic film made up of billions of E. coli bacteria that produced a pigment — or didn’t — depending on whether they were exposed to light. A few years later, he helped program the bacteria to detect the outlines of different objects within a single image, a complicated process known as edge detection.
Now Tabor is moving away from what he calls “toy projects” and using his experience to turn E. coli into medicine. He explained his research in an interview.
Let’s start with some background. What is the microbiome?
There are 100 trillion microbes living upon and within our bodies. That’s 10 microbes for every one of our own cells. They are on our skin, they are in our mouth, and a lot of them are in our stomach and intestine.
How do these microbes affect our health?
We’ve recently done a lot of mapping to figure out which microbes are where, and how sick people with different diseases have different microbes in different locations. It is looking more and more that our microbes not only play lots of essential roles in the metabolism and immune function in healthy people, but they can also be the origin of diseases. So if there is a disruption in some of these microbial communities, it can lead to a range of diseases, just like if you have a genetic mutation in your liver or heart.
I get that microbes can affect us physically, but how do they affect our mood?
There is something that researchers are calling the gut-brain axis. We think this happens via the vagus nerve, which connects your intestine to your brain. A recent study shows that the microbes inside your large intestine are sending signals to your brain, which affects anxiety and related behaviours. The researchers did an experiment with mice where they removed the vagus nerve, and the gut microbiome no longer affected the brain. It is also likely there are other connections through the fluids in your body.
You recently received a $500,000 (Dh1835,000) grant from the US Navy to create an E. coli that can fight obesity and anxiety. What does the microbiome have to do with obesity?
Not all obesity is caused the same way, but gut bacteria disruptions can cause obesity. Compelling studies show that putting gut bacteria from an obese human into a mouse causes the mouse to be obese. And that’s whether the mouse is fed a healthy low-fat diet or an unhealthy diet.
What is even more amazing is if you take the gut bacteria from the lean twin of an obese human and put it in a separate mouse, that mouse stays lean. And it even gets crazier: If the obese mouse is put in the same cage with a lean mouse, they will share gut bacteria because mice eat each other’s poop. Over time, the obese mouse becomes lean because it gets the lean bacteria. It turns out those lean bacteria are healthier and more invasive and can take over.
That is insane! So how will your E. coli get unhealthy guts back to healthy again?
Just last year, a nice study came out where the researchers did metabolic profiling in the large intestine. So far they found about 30 metabolites that were at elevated levels in obese guts and about 20 that were elevated in lean guts. They are like chemical signatures that are linked to this diseased state. We want to deliver a genetically engineered probiotic that can detect the early molecular signatures of a disrupted gut microbiome. Then, when that signature is detected, our bacteria will produce a battery of different compounds that prevents the changes in the intestine that lead to obesity and anxiety.
What are you going to do to the E. coli to turn it into a smart medicine?
Our research area is synthetic biology. We program living organisms just like you program a robot or a computer, but we are programming them with genes. We connect genes taken from nature in different kinds of ways in order to rationally design a new genetic circuit that controls what the E. coli does. We basically leave the organism mostly as it is, but we get rid of features we don’t want and add features we do want. The core of the organism is still there.
Why do you think the Navy was interested in funding this research?
The basic health and performance of soldiers in combat situations is a really big area of concern for the Navy. There is a whole set of mental and physical problems that they would like to learn to overcome. For example, traveller’s diarrhoea is a big problem for the Navy and the entire military. It costs them a lot of resources and time. We are solving weight gain and anxiety, which can also reduce the effectiveness of midshipmen when they are in the field.
Has anyone done anything like this before?
Yes, a few people have done pieces of what we are proposing. Some of the most exciting work is from John March at Cornell University, who has engineered a probiotic E. coli that reduces the instance of cholera in mice by 77 per cent. The E. coli produces a chemical that jams the communication channel that Vibrio cholerae, the bacteria that cause cholera, use to coordinate an attack in your gut and make you sick.
More recently he engineered a probiotic E. coli that can treat Type 1 diabetes in mice. The E. coli secrete a protein that can convert the stem cells naturally in the intestine to act like pancreas-like cells that secrete insulin, so the intestine starts to act like a pancreas.
I have to ask: Doesn’t E. coli cause food poisoning?
There are bad E. coli and good E. coli, and we are starting with a probiotic strain that is a natural resident of your healthy gut.
How would people take this probiotic? A pill? A drink?
It can be any imaginable way. When we test it in a mouse, you can just feed it to a mouse via a feeding tube. But if a person were going to eat, it I’d say yogurt would be a good way.
We’ve talked about genetically modified E. coli treating anxiety, obesity, cholera and Type 1 diabetes. Do you think this method could work on other diseases as well?
There is so much known about the microbiome now that we are almost tripping all over ourselves with possibilities. I know we haven’t achieved anything yet, but it really feels like the tip of the iceberg. There are so many other diseases and examples we could come up with. It really does feel like we are at the future here.
–Los Angeles Times