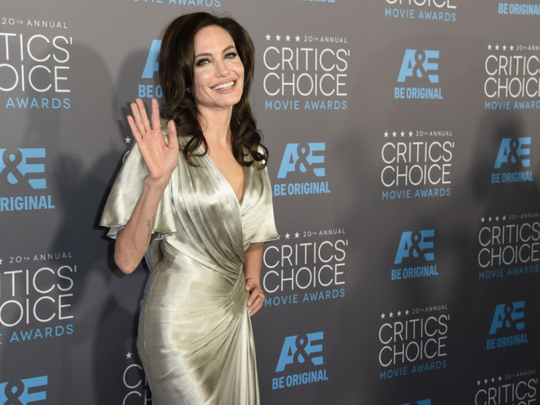
Angelina Jolie’s decision to remove her breasts, and most recently, her ovaries and Fallopian tubes, has been hailed as brave. But it all began with another major decision — to have genetic testing. While genetic testing may appear to be a modern medical miracle, a cancer doctor in the UAE on Tuesday warned against taking the decision to do genetic testing lightly.
Jolie on Tuesday announced the precautionary removal of her ovaries and Fallopian tubes, two years after removing her breasts, because she discovered through genetic testing that she is a carrier of the mutated BCRA1 gene, which can significantly increase the risk of breast and ovarian cancer. Her mother, grandmother and aunt died of cancer.
“People need to speak to professional counsellors, doctors, but most of all, people who actually underwent this kind of operation. Some people loved it, some people regret it. It is a life changer. They need to understand the consequences,” said Dr Sawsan Abdul Salam Al Madhi, secretary general of Friends of Cancer Patients. “People need to do proper counselling before getting tested, and after getting tested.”
Speaking on the final day of the Pink Caravan, a pan-UAE breast cancer awareness initiative that concluded at Zayed Military Hospital in Abu Dhabi, Dr Sawsan cautioned those inspired by Jolie’s actions to also make sure they are fully informed about the financial, legal and regulatory repercussions — such as whether a patient will still get insurance coverage. “One of our messages is dispelling the myths about cancer. And if you have any doubts, go and ask your doctor. Knowledge will always be the cornerstone.”
She cautioned that genetic testing is not a final word on cancer prediction. “Studies tell us genetics plays a huge role when it comes to increasing the risk, but when you see women who have breast cancer, almost 60-65 per cent don’t have any genetic mutation. The mutation increases the risk, but no one can guarantee if you will get it.”
“If you’ve got [the faulty gene] what does it mean? ‘I’m going to die?’ No, it doesn’t mean that. What does it mean if it’s negative? You won’t get breast cancer, you can go and enjoy the rest of your life? No, it doesn’t mean that. You have to go and get your check-up and screening, every year.”











